So you’ve heard about oxalates, those compounds found in certain foods that can form kidney stones if consumed in excessive amounts. But did you know that your body actually has an oxalate tolerance level? In this article, we will explore the concept of oxalate tolerance and why it’s essential to understand how much oxalate your body can handle. Whether you’re curious about your own tolerance or simply seeking ways to improve your overall health, uncovering the truth about oxalate tolerance is a must-read.

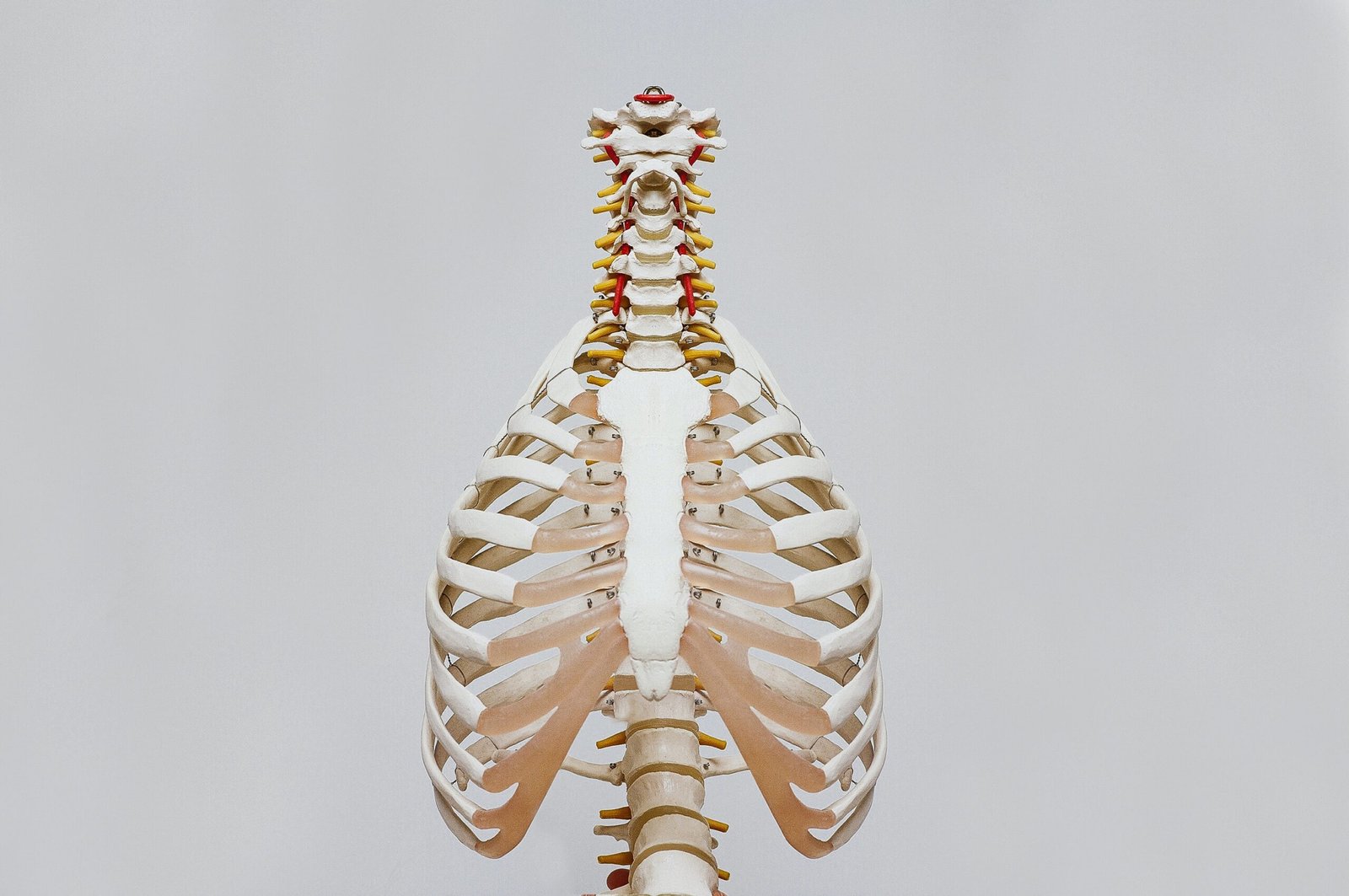
This image is property of images.unsplash.com.
Overview
What is Oxalate Tolerance?
Oxalate tolerance refers to a person’s ability to handle and metabolize oxalates, which are natural compounds found in certain foods. Oxalates can bind to minerals like calcium and form crystals, which can then lead to the formation of kidney stones. People with poor oxalate tolerance may experience symptoms such as digestive issues, musculoskeletal problems, and urinary difficulties.
Importance of Oxalate Tolerance
Having good oxalate tolerance is essential for maintaining overall health, as it helps prevent the formation of kidney stones and other related complications. By understanding the causes, symptoms, diagnosis, and management of oxalate intolerance, individuals can take proactive steps to reduce oxalate intake and prevent potential complications.
Causes of Poor Oxalate Tolerance
Genetic Factors
Certain genetic factors can contribute to poor oxalate tolerance. People with a family history of oxalate-related conditions such as hyperoxaluria or kidney stones may have a higher risk of developing oxalate intolerance due to inherited genetic variations.
Dietary Factors
Consuming a diet high in oxalate-rich foods can increase the risk of developing oxalate intolerance. Foods such as leafy greens, nuts and seeds, beets, chocolate, and tea are known to have high oxalate content. Consuming these foods in excessive amounts or as a significant part of one’s diet can overwhelm the body’s ability to metabolize oxalates effectively.
Gut Health
An unhealthy gut can also contribute to poor oxalate tolerance. The gut microbiome plays a crucial role in metabolizing oxalates. Imbalances in gut bacteria and certain health conditions that affect gut health, such as inflammatory bowel disease or antibiotic use, can disrupt the proper breakdown and elimination of oxalates from the body.
Other Medical Conditions
Certain medical conditions can be associated with poor oxalate tolerance. These include primary hyperoxaluria, Crohn’s disease, celiac disease, and vitamin B6 deficiency. These conditions can either increase the production of oxalates in the body or impair the body’s ability to metabolize them effectively.
This image is property of images.unsplash.com.
Symptoms of Oxalate Intolerance
Digestive Symptoms
Digestive symptoms associated with oxalate intolerance may include abdominal pain, bloating, gas, diarrhea, or constipation. These symptoms often occur due to the formation of oxalate crystals in the gastrointestinal tract, leading to irritation and inflammation.
Musculoskeletal Symptoms
Musculoskeletal symptoms of oxalate intolerance can include joint pain, muscle stiffness, or general discomfort. These symptoms may arise due to the deposition of oxalate crystals in the joints or muscles, causing inflammation and pain.
Urinary Symptoms
Urinary symptoms associated with oxalate intolerance primarily revolve around kidney health. Increased levels of oxalates in the urine can contribute to the formation of kidney stones, leading to symptoms such as pain in the lower back or sides, blood in the urine, or frequent urination.
Other Symptoms
Oxalate intolerance can also manifest in other ways. Some individuals may experience fatigue, headaches, skin issues, or even mood disturbances. These symptoms can be attributed to the body’s inability to effectively process and eliminate oxalates, resulting in systemic inflammation and oxidative stress.
Diagnosis of Oxalate Intolerance
Medical History and Physical Examination
During the diagnosis of oxalate intolerance, healthcare professionals will typically gather a detailed medical history and perform a physical examination. This helps them assess potential risk factors, evaluate symptoms, and rule out other underlying conditions. Be prepared to provide information about your dietary habits, family history, and any past or present medical conditions.
Urinary Oxalate Testing
Urinary oxalate testing is a common diagnostic method for oxalate intolerance. This involves analyzing a urine sample to measure the levels of oxalates excreted by the body. Elevated urinary oxalate levels can indicate poor oxalate tolerance and increased risk of kidney stone formation.
Elimination Diet
An elimination diet may be recommended to determine if certain high-oxalate foods are triggering symptoms. The diet involves temporarily eliminating foods high in oxalates and gradually reintroducing them while monitoring for reactions. This process can help identify specific foods that may be contributing to oxalate intolerance.
Other Diagnostic Tests
Depending on the individual case, additional diagnostic tests may be necessary. These can include blood tests to assess kidney function, imaging tests like ultrasounds or CT scans to evaluate the presence of kidney stones, or genetic testing to identify any underlying genetic factors contributing to poor oxalate tolerance.

This image is property of images.unsplash.com.
Management of Oxalate Intolerance
Low-Oxalate Diet
One of the primary ways to manage oxalate intolerance is through a low-oxalate diet. This involves limiting or avoiding foods high in oxalates. Some examples of high-oxalate foods include leafy greens, nuts and seeds, beets, chocolate, and tea. By reducing intake of these foods and opting for low-oxalate alternatives, individuals can help minimize oxalate-related symptoms.
Calcium Supplementation
Calcium supplementation can help prevent the absorption of oxalates in the gut by binding to them and forming insoluble complexes. It is important to consult with a healthcare professional before taking calcium supplements to determine the appropriate dosage and avoid potential interactions with other medications.
Increase Hydration
Staying adequately hydrated is crucial for managing oxalate intolerance. Drinking plenty of fluids, especially water, can help dilute the concentration of oxalates in the urine and promote their excretion. Aim to drink at least 8 glasses of water per day, and more if engaging in physical activity or in hot weather.
Probiotics and Gut Health
Maintaining a healthy gut microbiome is essential for effective oxalate metabolism. Probiotics, which are beneficial bacteria, can help restore and maintain a healthy balance of gut flora. Including probiotic-rich foods like yogurt and fermented vegetables or taking probiotic supplements may be beneficial for improving gut health and reducing oxalate-related symptoms.
Medications
In some cases, medications may be prescribed to manage oxalate intolerance. These can include medications that bind to oxalates in the gut, such as calcium citrate or cholestyramine, or medications that reduce oxalate production in the body, such as pyridoxine (vitamin B6). The specific medication and dosage will depend on individual circumstances and should be determined by a healthcare professional.
Foods High in Oxalates
Leafy Greens
Leafy greens such as spinach, kale, and Swiss chard are notoriously high in oxalates. While they offer many health benefits, individuals with oxalate intolerance should consume them in moderation or consider alternatives.
Nuts and Seeds
Certain nuts and seeds, including almonds, cashews, and sesame seeds, have a high oxalate content. Individuals with oxalate intolerance should be mindful of their intake and opt for low-oxalate alternatives.
Beets
Beets are rich in oxalates and can contribute to oxalate-related symptoms. Those with poor oxalate tolerance may need to limit their consumption or explore alternatives.
Chocolate
Chocolate, especially dark chocolate, contains significant amounts of oxalates. While it may be tempting, those with oxalate intolerance should exercise caution and consume in moderation.
Tea
Tea, such as black tea and green tea, is another common source of oxalates. Limiting tea consumption or exploring herbal tea options with lower oxalate content may be advisable for individuals with oxalate intolerance.
Other Foods
Other foods that can be high in oxalates include certain fruits (such as raspberries and figs), grains (such as buckwheat and quinoa), and legumes (such as soybeans and baked beans). It is important to be mindful of the oxalate content in these foods and consider alternatives if necessary.
Foods Low in Oxalates
Root Vegetables
Root vegetables like carrots, sweet potatoes, and parsnips are generally low in oxalates and can be enjoyed as part of a low-oxalate diet.
Fruits
Many fruits have a lower oxalate content and can be included in the diet of individuals with oxalate intolerance. These include apples, pears, grapes, and melons. However, it is important to limit or avoid fruits like raspberries or figs, which are higher in oxalates.
Grains
Some grains, such as rice, oats, and corn, have a lower oxalate content and can be included in a low-oxalate diet. However, certain grains like buckwheat and quinoa should be consumed in moderation due to their higher oxalate content.
Dairy Products
Most dairy products, including milk, cheese, and yogurt, are generally low in oxalates and can be enjoyed as part of a low-oxalate diet. However, individuals with lactose intolerance or dairy allergies should opt for dairy alternatives.
Lean Meats
Lean meats like chicken, turkey, and fish are generally low in oxalates and can be a good source of protein for individuals with oxalate intolerance. It is important to choose lean cuts and avoid processed meats, which may contain additives.
Other Foods
Other foods low in oxalates include eggs, tofu, certain herbs and spices, and certain types of fish (such as salmon and trout). These foods can be included in a low-oxalate diet to provide variety and nutrition.
Tips for Reducing Oxalate Intake
Cooking Techniques
Certain cooking techniques can help reduce the oxalate content in foods. Boiling, steaming, or blanching vegetables can decrease their oxalate levels. Additionally, soaking high-oxalate grains and legumes overnight before cooking can leach out some of the oxalates.
Food Preparation Methods
Peeling and deseeding fruits and vegetables can help reduce oxalate content. Removing the skin and seeds of high-oxalate foods like tomatoes or cucumbers can decrease the overall oxalate intake.
Portion Control
While consuming low-oxalate foods is important, portion control is equally vital. Moderation is key to ensure a balanced intake of nutrients and to avoid excessive consumption of any particular food.
Reading Food Labels
Familiarize yourself with reading food labels to identify the oxalate content of packaged and processed foods. Look for ingredients like spinach, almonds, or cocoa that may indicate higher oxalate levels.
Choosing Low-Oxalate Alternatives
When following a low-oxalate diet, it is essential to find suitable alternatives for high-oxalate foods. For example, opting for cauliflower rice instead of traditional rice or using zucchini noodles instead of pasta can help reduce oxalate intake while still enjoying a variety of flavors.
Potential Complications of Oxalate Intolerance
Kidney Stones
The formation of kidney stones is one of the most significant complications associated with poor oxalate tolerance. Kidney stones can cause severe pain and other urinary symptoms. Managing oxalate intake and following medical advice can help reduce the risk of kidney stone formation.
Nutrient Deficiencies
Restricting or eliminating high-oxalate foods from the diet can lead to nutrient deficiencies if not adequately substituted. It is important to ensure a well-balanced and varied diet that provides all essential nutrients.
Impact on Bone Health
High levels of urinary oxalates can contribute to the development of osteoporosis or weakened bones over time. Adequate calcium intake, along with other bone-strengthening strategies, is crucial for individuals with oxalate intolerance to protect their bone health.
Frequently Asked Questions
Can Oxalate Intolerance be Cured?
Oxalate intolerance cannot be fully cured, but with proper management, individuals can effectively control symptoms and reduce the risk of complications. Following a low-oxalate diet, maintaining good hydration, and managing underlying medical conditions can significantly improve quality of life.
Is Oxalate Intolerance Common?
Oxalate intolerance is relatively common, but the severity and prevalence of symptoms can vary widely among individuals. It is important to consult with a healthcare professional to determine the appropriate course of action based on one’s specific situation.
Can Oxalate Intolerance Develop Later in Life?
While oxalate intolerance can be present from birth due to genetic factors, it can also develop later in life. Factors such as dietary changes, gut health issues, or the onset of certain medical conditions can contribute to the development of oxalate intolerance in adulthood. Regular monitoring, early diagnosis, and proper management are essential in such cases.
In conclusion, understanding and managing oxalate tolerance is vital for maintaining overall health and preventing complications. By identifying the causes, recognizing the symptoms, and following appropriate diagnostic and management strategies, individuals can effectively mitigate the impact of oxalate intolerance and promote better well-being.