Have you ever wondered how the tiny inhabitants of your gut influence your overall health? It’s fascinating and a bit overwhelming to think about, isn’t it? One particular area that’s been getting a lot more buzz lately is the relationship between your gut microbiome and oxalate sensitivity.

What is the Gut Microbiome?
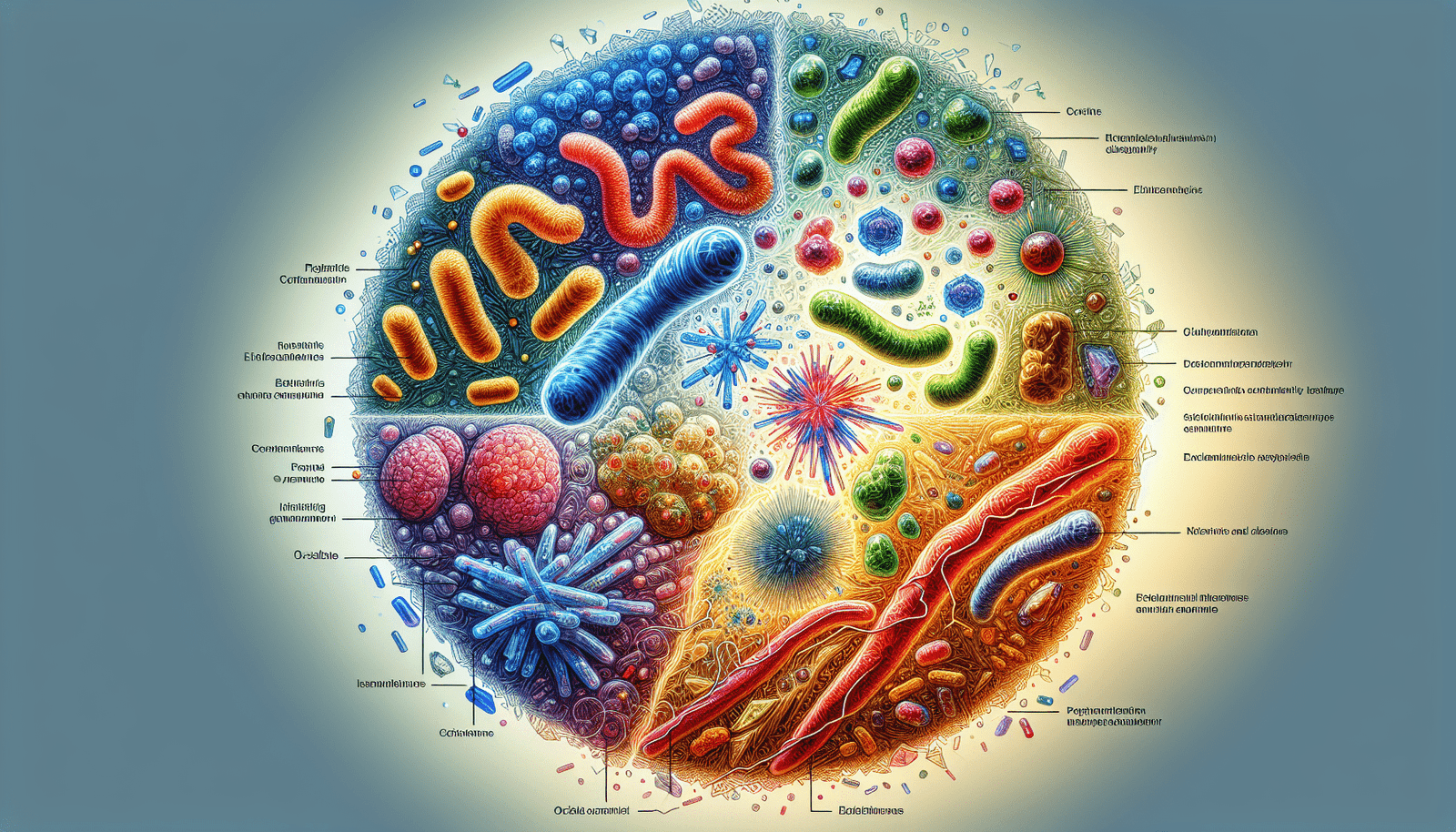
The gut microbiome sounds pretty scientific, but it’s essentially the collection of trillions of microorganisms hanging out in your digestive tract. These include bacteria, viruses, fungi, and other microscopic critters that play an essential role in your digestive and immune systems. Think of them as a bustling community where each resident has a specific job that helps maintain your overall health. The balance and types of microorganisms can affect everything from how well you digest food to how your immune system responds to threats.
How Does the Gut Microbiome Work?
Imagine your gut as a complex ecosystem, much like a forest. Multiple species of trees, plants, and animals coexist and help each other survive. In your gut, beneficial bacteria break down food particles, extract nutrients, and even produce essential vitamins like B12 and K. If this ecosystem is thrown off balance—let’s say a wildfire sweeps through—harmful bacteria can then overpopulate, and that’s when problems start to occur.
The Importance of a Balanced Gut
Why is a balanced gut so crucial? When your gut microbiome is in harmony, it helps to combat harmful pathogens, supports digestion, and even impacts your mental health. Yes, your gut and brain are so intertwined that the gut is often called your “second brain.” An imbalance can lead to various health problems like inflammatory bowel diseases, allergies, and perhaps even influence your susceptibility to oxalate sensitivity.
Understanding Oxalates
Before diving deeper into oxalate sensitivity, you might be curious to know what oxalates are. Oxalates are natural compounds found in many plant-based foods. They bind with minerals like calcium to form crystals, often staying soluble in the gut and getting eliminated from the body through urine.
Foods High in Oxalates
Here’s a short table to give you a quick rundown of some common foods rich in oxalates:
| Food | Oxalate Content (mg per serving) |
|---|---|
| Spinach | 755 |
| Beet Greens | 916 |
| Rhubarb | 541 |
| Almonds | 122 |
| Sweet Potatoes | 114 |
| Dark Chocolate | 117 |
| Berries | Varies (20-50) |
As you can see, foods high in oxalates are often those we consider healthy. That’s why it’s essential to understand how these compounds interact with your body.
Oxalate Sensitivity and Its Symptoms
So, what’s the big deal about oxalates? For most people, consuming foods high in oxalates isn’t a problem. However, for those with oxalate sensitivity, these compounds can form crystals in the body, leading to issues like kidney stones, joint pain, and even some forms of vulvodynia. Symptoms can range from digestive discomfort to more severe manifestations like painful urinary symptoms or fibromyalgia-like pain.
The Connection Between Gut Microbiome and Oxalate Sensitivity
How does your gut microbiome influence oxalate sensitivity? It’s all about balance. Certain beneficial bacteria in your gut can help break down oxalates before they can form harmful crystals. For instance, Oxalobacter formigenes is a bacterium that specifically degrades oxalates, thereby reducing the chances of oxalate-related issues.
The Role of Oxalobacter formigenes
Oxalobacter formigenes is like the janitor of your digestive tract, specialized in cleaning up oxalates. The more of these bacteria you have, the better your gut can manage and eliminate oxalates naturally. Unfortunately, factors like antibiotic use, diet, and lifestyle can reduce this beneficial population.
Impact of Antibiotics and Diet
Imagine you have a garden full of beautiful flowers, but one day, you indiscriminately spread weed killer everywhere. This might kill harmful weeds but also harm your precious flowers. That’s what happens when you take antibiotics—they don’t discriminate between good and bad bacteria. A course of antibiotics can significantly reduce your beneficial bacteria, including the oxalate-degrading Oxalobacter formigenes. Similarly, a poor diet loaded with processed foods and low in fiber can disrupt your gut’s balance, making it less effective at handling oxalates.
Strategies for Managing Oxalate Sensitivity
If you suspect you’re sensitive to oxalates, there are strategies you can consider to help manage your symptoms.
Probiotics and Prebiotics
Start with your gut. Introducing probiotics and prebiotics can help restore the balance of beneficial bacteria. Probiotics are live beneficial bacteria, while prebiotics are types of fiber that feed these good bacteria. Foods like yogurt, kefir, and fermented vegetables are good sources of probiotics. Prebiotics can be found in foods like garlic, onions, and bananas.
Dietary Adjustments
Watching what you eat can make a big difference. If you discover you’re sensitive to oxalates, consider adjusting your diet to limit oxalate-rich foods. It doesn’t mean you have to completely avoid foods like spinach or almonds, but moderation is key. Drinking plenty of water can also help as it dilutes the oxalates and aids in their excretion.
Supplements
There are also specific supplements that may help with oxalate sensitivity. For example, calcium supplements taken with meals can bind to oxalates in the gut and help prevent them from being absorbed into your bloodstream. Other supplements like magnesium and potassium citrate may also help.
Medical Interventions
In severe cases, medical interventions might be necessary. If you’re forming kidney stones frequently or experiencing severe symptoms, consult a healthcare provider for treatments like medications that inhibit oxalate absorption.

The Future of Gut Health and Oxalate Sensitivity
What’s on the horizon for this field? More research is continuously being conducted to better understand the complex relationship between our gut microbiota and various health conditions, including oxalate sensitivity.
The Promise of Personalized Medicine
Imagine a future where your medical treatment is tailored specifically to your unique genetic makeup and microbiome composition. Personalized medicine is an exciting development where you might one day have specific treatments or dietary plans customized just for you. The hope is that by understanding more about our microbiomes, we can create more effective, individualized treatments for conditions like oxalate sensitivity.
Advanced Probiotic Treatments
Scientists are also working on advanced probiotics designed to deliver beneficial bacteria more effectively. One day, you might take a specialized probiotic that not only restores your gut flora but also boosts your oxalate-degrading bacteria, offering a more targeted approach to managing sensitivity.

Conclusion
Navigating the complex interplay between your gut microbiome and oxalate sensitivity can feel like a lot to handle. However, understanding how these factors influence your health can empower you to make better choices. Remember, a balanced gut is crucial, not just for managing oxalate sensitivity but for overall well-being. Whether it’s through diet, supplements, or future medical advancements, there are multiple ways to maintain that balance. So next time you munch on a handful of spinach or savor a piece of dark chocolate, you’ll have a bit more insight into what’s happening on a microscopic level in your body.