Have you ever found yourself struggling with heartburn or those annoying, relentless symptoms of gastroesophageal reflux disease (GERD), only to wonder where they came from?

Understanding Gastroesophageal Reflux
Gastroesophageal reflux occurs when stomach acid flows back into the esophagus, causing discomfort and a variety of unpleasant symptoms. You might notice a burning sensation in your chest or throat, regurgitation of food or sour liquid, difficulty swallowing, or even a persistent cough. It’s more than just a nuisance; it can affect your daily life and overall well-being.
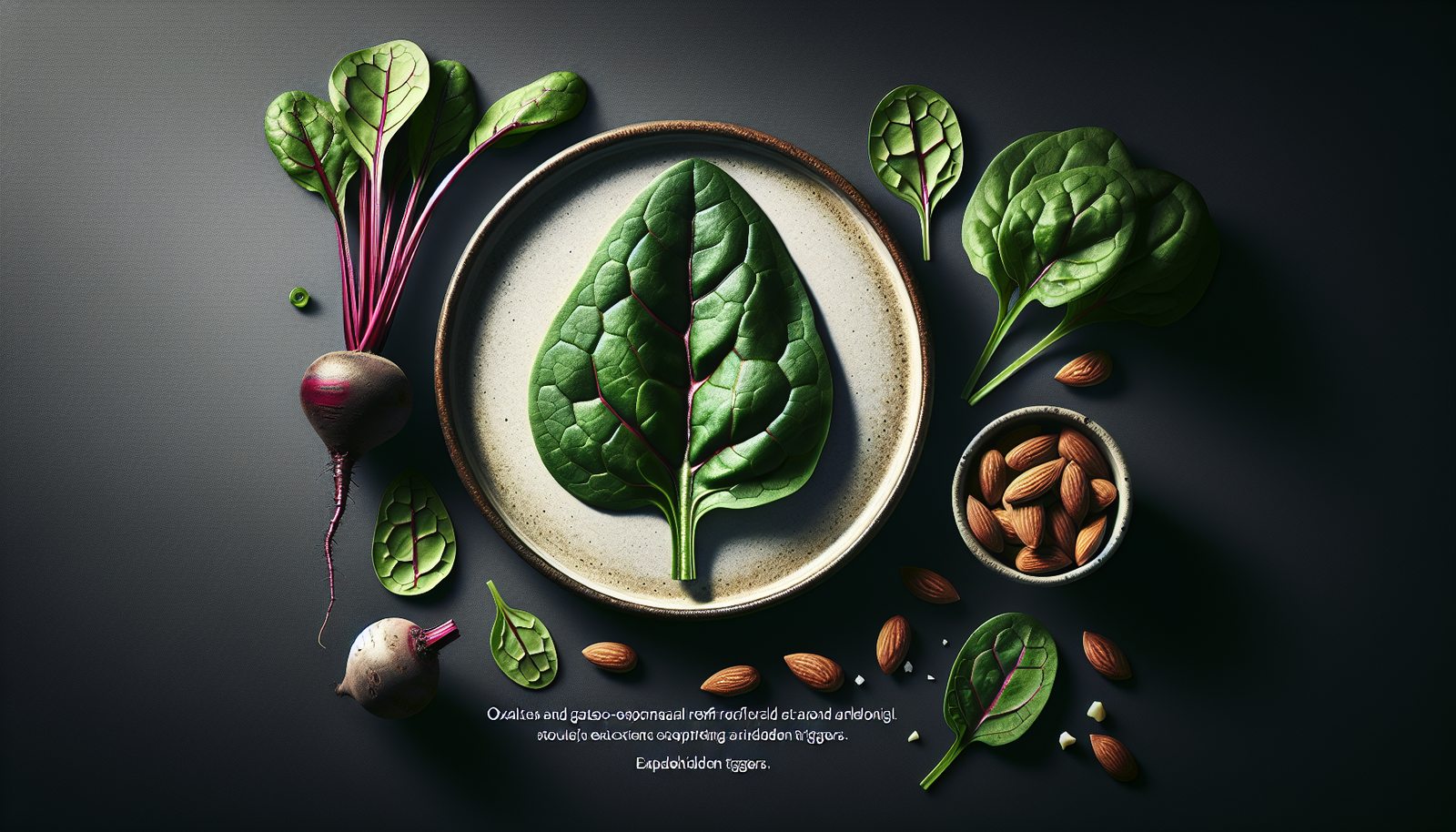
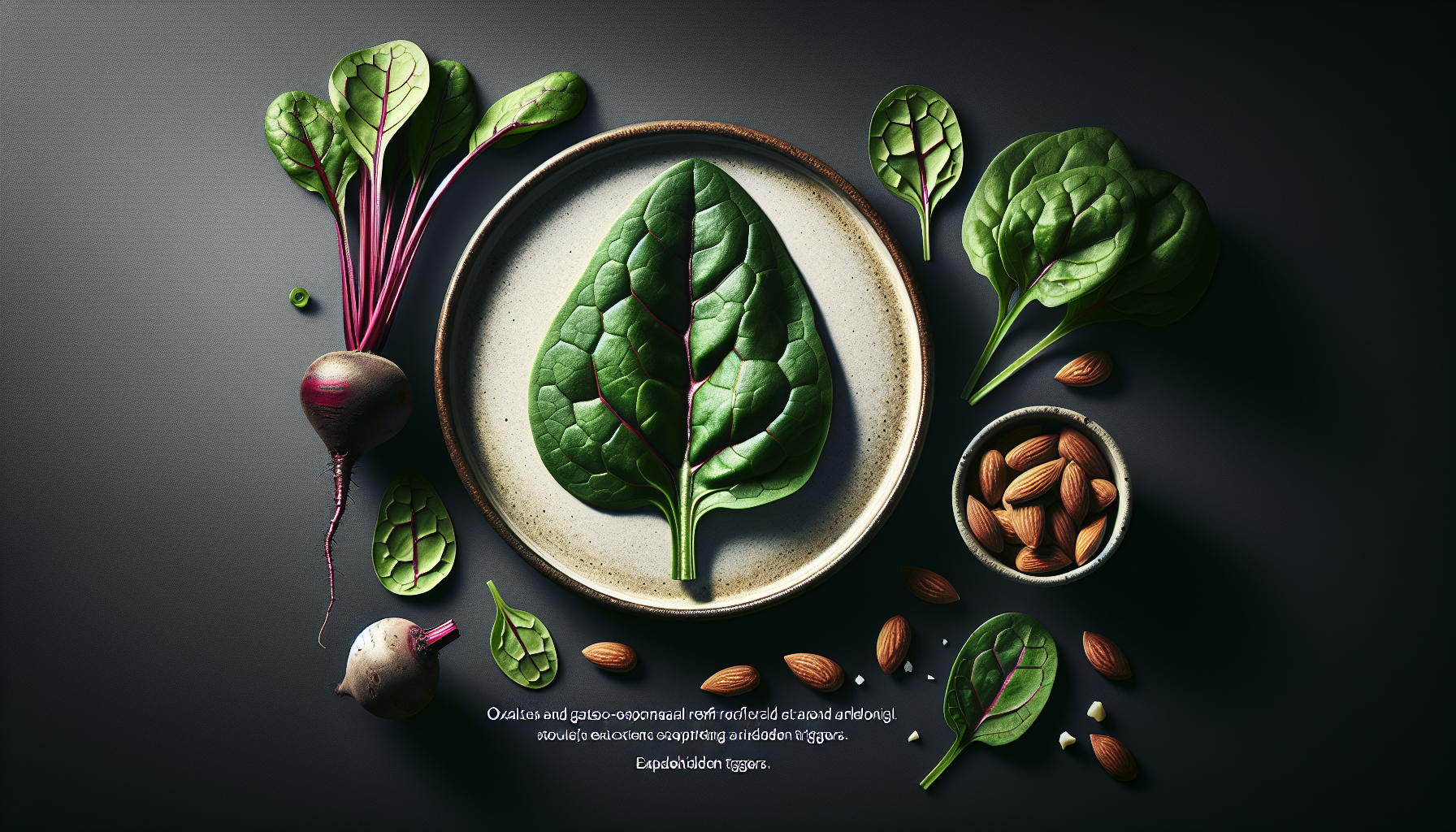
What if I told you that some seemingly innocent foods could be exacerbating your symptoms? One category of food that’s often overlooked in the discussion of GERD is high-oxalate foods. Let’s delve into how oxalates could potentially influence your experience with gastroesophageal reflux.
What Are Oxalates?
Oxalates are naturally occurring compounds found in many plants, especially leafy greens, nuts, and certain fruits. While they play a role in plant metabolism, oxalates can also bind to minerals like calcium, potentially forming insoluble compounds. For some individuals, especially those prone to kidney stones, high oxalate levels can be a concern. But the connection between oxalates and gastroesophageal reflux is less well known.
High-Oxalate Foods
If you’re wondering whether you consume high-oxalate foods, here’s a table that breaks it down:
| Food Category | High-Oxalate Foods |
|---|---|
| Leafy Greens | Spinach, Swiss chard, Beet greens |
| Nuts and Seeds | Almonds, Cashews, Peanuts |
| Vegetables | Rhubarb, Sweet potatoes, Potatoes |
| Fruits | Starfruit, Blackberries, Cranberries |
| Grains | Wheat bran, Buckwheat |
Keeping an eye on the foods you consume can help you identify any potential triggers for your reflux symptoms.
Why Oxalates Might Matter
Oxalates might be a hidden trigger for your gastroesophageal reflux symptoms for a few reasons. First, some high-oxalate foods are also high in acidity or can lead to increased stomach acid production. When you combine high acidity and oxalates, you might just be setting the stage for a flare-up of reflux symptoms.
The acidic nature of certain oxalate-rich foods
Many high-oxalate foods, particularly leafy greens and certain fruits, also possess acidic properties or can stimulate gastric acid secretion, which can irritate your esophagus. You could be indulging in what you believe are “healthy” foods, yet inadvertently aggravating your reflux.
Symptoms You Might Experience
Pay attention to your body after consuming high-oxalate foods. If you notice symptoms like:
- Increased heartburn
- A sour taste in your mouth
- Nausea or a feeling of fullness
These could be warning signs that oxalates are playing an unexpected role in your gastroesophageal reflux issues.

Other Common Triggers of GERD
While our focus is on oxalates, it’s worth noting that other common triggers of GERD exist. Understanding these can help you take a more comprehensive approach to managing your symptoms. Here are some well-known culprits:
| Common Triggers | Description |
|---|---|
| Fatty Foods | Slow gastric emptying, leading to excessive acid production |
| Caffeine | Relaxes the lower esophageal sphincter (LES) |
| Alcohol | Increases stomach acid; irritates the esophagus |
| Spicy Foods | Can directly irritate the gastrointestinal tract |
| Chocolate | Contains methylxanthines, which can relax the LES |
It’s crucial to identify your personal triggers, as they might not be the same for everyone.
Identifying Your Triggers
You might be wondering: how can you effectively pinpoint your GERD triggers, including oxalates? Consider this step-by-step approach:
-
Keep a Food Diary: Start writing down everything you eat and drink, along with any symptoms you experience. Keep it for at least a week.
-
Reduce Portion Sizes: Sometimes it’s not just about what you eat, but how much. Starting with smaller portions might alleviate symptoms.
-
Eliminate Problematic Foods: If you suspect high-oxalate foods are causing issues, consider reducing or eliminating them for a few weeks to see if your symptoms improve.
-
Reintroduce Foods Slowly: After a break, gradually reintroduce foods to see if any specifically trigger symptoms.
-
Consult a Nutritionist or Healthcare Provider: They can help you navigate your food choices in a more informed way.

Managing Oxalate Intake
Managing your oxalate intake doesn’t mean you have to eliminate all high-oxalate foods. Here’s how you can strike a balance:
Portion Control
You don’t need to forego your favorite greens, but moderating your intake can help. For example, instead of large servings of spinach, consider mixing it with lower-oxalate greens like kale or lettuce.
Cook Your Greens
Cooking can significantly reduce the oxalate content in some foods. Steaming spinach or Swiss chard can leach out some of those pesky oxalates, making them less likely to irritate your system.
Seeking Alternatives
If you’ve decided high-oxalate foods are not your friend, what can you eat instead? Fortunately, many tasty alternatives exist.
| Lower-Oxalate Alternatives | Examples |
|---|---|
| Leafy Greens | Romaine lettuce, Kale, Cabbage |
| Vegetables | Zucchini, Bell peppers, Broccoli |
| Fruits | Apples, Bananas, Blueberries |
| Grains | White rice, Quinoa |
Switching out high-oxalate foods for these options can provide relief while still allowing you to enjoy a varied and nutritious diet.
The Role of Hydration
Hydration plays a significant role in managing GERD and oxalate levels in the body. Drinking enough water can help dilute stomach acid and may help minimize reflux symptoms. Also, it’s important for kidney health, which can be affected by high oxalate intake.
How Much Water Should You Drink?
The general recommendation is to aim for about 8 cups (64 ounces) of water per day, but individual needs vary. If you’re active or live in a hot climate, you might need more.
Lifestyle Changes to Consider
Managing GERD may not only be about what you eat, but also about how you live. Here are a few tips to enhance your lifestyle:
Elevate Your Head While Sleeping
Sleeping with your head elevated can help reduce nighttime reflux. Try adding a wedge pillow to keep your upper body elevated.
Maintain a Healthy Weight
Extra weight, especially around the abdomen, can increase the pressure on your stomach, pushing acid back up into the esophagus. If weight loss is a goal for you, combining a balanced diet with regular physical activity can help.
Practice Stress Management
Stress can exacerbate digestive issues. Find relaxing activities that resonate with you, whether it’s yoga, meditation, or simply taking a leisurely walk.

Seeking Medical Guidance
If you’re tirelessly trying to manage your symptoms but nothing seems to work, it might be time to consult a healthcare provider. They can offer more tailored approaches. Depending on your symptoms, a possible referral to a gastroenterologist for further evaluation might be warranted.
Medical Treatments for GERD
There are several options available, including:
- Antacids: Quick relief for heartburn, but they don’t heal the esophagus.
- H2 Blockers: Reduce acid production and help heal the esophagus.
- Proton Pump Inhibitors (PPIs): Effective for frequent heartburn, but long-term use should be monitored by a physician.
While you’re focusing on nutrition and lifestyle, medical treatment can provide additional support as you navigate your symptoms.
Conclusion
The journey to uncovering your personal triggers can feel overwhelming, but understanding the connection between oxalates and gastroesophageal reflux may provide you with newfound insights. By keeping a close eye on your diet, exploring alternatives, and making lifestyle changes, you might just find a path that reduces your reflux symptoms and improves your overall quality of life.
Take control of your health. Each small change you implement can lead to significant benefits over time. Remember, you’re not alone in this; you’re on a journey toward understanding your body better and making informed choices for your well-being.