Have you considered how dietary oxalates might be affecting your experience of menopause? As you navigate this stage of life, understanding and managing your intake of oxalates can be crucial to your overall health and well-being. Oxalates, organic compounds found in many plant foods, can contribute to various health issues, particularly during menopause, when changes in hormone levels might make you more susceptible to certain conditions.
Understanding Oxalates
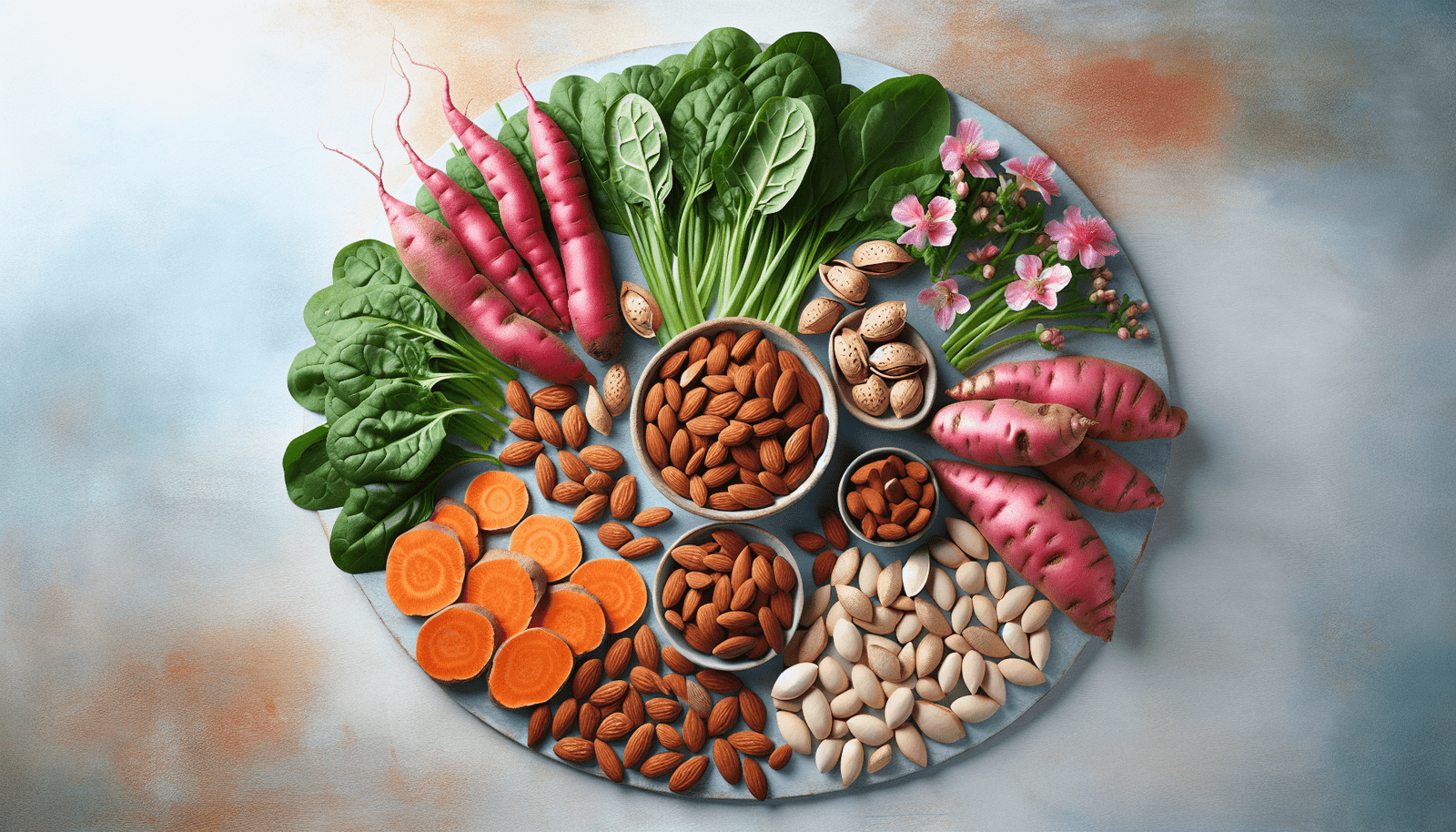
Oxalates are naturally occurring compounds in many foods, especially plant-based ones. While they play a role in plant metabolism, they can sometimes pose health risks to humans. When consumed in large amounts, oxalates can interfere with mineral absorption and contribute to the formation of kidney stones.
Oxalate-rich foods include:
| High-Oxalate Foods | Oxalate Content (mg/100g) |
|---|---|
| Spinach | 750 |
| Rhubarb | 600 |
| Beets | 150 |
| Almonds | 450 |
| Sweet Potatoes | 100 |
How Oxalates Affect Your Health
Oxalates can bind to minerals like calcium, forming insoluble compounds. These compounds are not easily absorbed by your body and can accumulate in the kidneys, leading to the formation of kidney stones. Additionally, high oxalate levels can potentially aggravate conditions such as vulvodynia, a condition that can be more pronounced during menopause due to hormonal changes.
Menopause and Oxalate Sensitivity
During menopause, your body’s hormonal balance shifts dramatically. Estrogen levels decrease, which can lead to increased calcium excretion. This loss of calcium can exacerbate the effects of oxalate consumption, making you more susceptible to kidney stones and other related issues.
Tips for Managing Oxalates
Effectively managing your oxalate intake involves dietary adjustments and other lifestyle changes that can help mitigate the risks. Here are some strategies you might find useful:
Moderating Oxalate-Rich Foods
While it’s not necessary to eliminate oxalate-containing foods entirely, moderation is key. Here’s a list of substitutions for high-oxalate foods:
| High-Oxalate Foods | Low-Oxalate Substitutes |
|---|---|
| Spinach | Kale, Cabbage |
| Rhubarb | Apples, Pears |
| Almonds | Pumpkin Seeds, Sunflower Seeds |
| Beets | Carrots, Cucumbers |
| Sweet Potatoes | White Potatoes |
Cooking Techniques to Reduce Oxalates
Certain cooking methods can help reduce the oxalate content in foods. Boiling vegetables, for example, can decrease oxalate levels significantly as oxalates leach into the boiling water, which you can then discard.
| Cooking Method | Effect on Oxalates |
|---|---|
| Boiling | Decreases oxalates |
| Steaming | Slightly decreases oxalates |
| Baking | No effect |
| Raw | No effect |
Ensuring Adequate Calcium Intake
Calcium can bind to oxalates in your digestive tract, reducing their absorption and subsequent risk of kidney stone formation. Therefore, consuming adequate amounts of calcium is crucial. Dairy products, fortified plant-based milks, and calcium-rich leafy greens like broccoli can be beneficial.
Staying Hydrated
Proper hydration helps to dilute your urine, decreasing the concentration of oxalates and other compounds that can contribute to kidney stone formation. Aim to drink at least 8-10 glasses of water daily.
Considering Probiotics
Certain probiotics can aid in degrading oxalates in your gut, thereby reducing their absorption. Foods like yogurt, kefir, and kombucha are not only rich in probiotics but also enhance gut health, which can be especially beneficial as you navigate menopause.

Integrating Lifestyle Changes
Managing oxalates during menopause isn’t solely about dietary adjustments; your overall lifestyle plays a significant role.
Regular Physical Activity
Engaging in regular physical activity helps improve calcium balance in your bones, reducing the excretion of calcium through urine. Aim for at least 150 minutes of moderate-intensity exercise per week.
Stress Management
Chronic stress can exacerbate hormonal imbalances and worsen symptoms of menopause. Practices like yoga, meditation, and deep breathing exercises can help you manage stress effectively.
Regular Medical Check-ups
Regular consultations with your healthcare provider can help monitor your health and adjust your diet and lifestyle as needed. Blood tests, urine tests, and imaging studies can provide insights into your oxalate levels and kidney function.
Personalized Nutrition Counseling
Working with a registered dietitian can help you develop a personalized nutrition plan that accommodates your specific needs during menopause. They can provide tailored advice and monitor your progress to ensure optimal health outcomes.
Foods to Embrace and Avoid
Creating a balanced diet that supports your overall health during menopause involves understanding which foods to embrace and which to limit based on their oxalate content.
Foods to Embrace
| Food Group | Examples | Benefits |
|---|---|---|
| Low-Oxalate Veggies | Kale, Cauliflower, Cucumbers | Rich in vitamins and minerals |
| Fruits | Apples, Bananas, Blueberries | Provide antioxidants and fiber |
| Protein Sources | Chicken, Tofu, Tuna | Essential for muscle maintenance |
| Whole Grains | Brown Rice, Quinoa, Oats | High in fiber and nutrients |
| Dairy/Alternatives | Milk, Cheese, Fortified Almond Milk | Rich in calcium |
Foods to Avoid
| Food Group | Examples | Drawbacks |
|---|---|---|
| High-Oxalate Veggies | Spinach, Swiss Chard, Beets | High in oxalates |
| Nuts and Seeds | Almonds, Sesame Seeds, Peanuts | High in oxalates and calories |
| Certain Fruits | Figs, Kiwi, Blackberries | High in oxalates |

Supplements and Medications
In some cases, dietary changes alone may not be sufficient to manage oxalate levels effectively. Supplements and medications might be necessary and should be discussed with your healthcare provider.
Calcium Supplements
If you find it challenging to get enough calcium through diet alone, calcium supplements might be recommended. Calcium citrate is often preferred, as it can prevent stone formation without increasing the risk of hypercalcemia.
Vitamin B6
Vitamin B6 has been shown to reduce oxalate production in some individuals. Foods rich in Vitamin B6, such as chickpeas, salmon, and potatoes, or supplements can be helpful.
Magnesium
Magnesium can also help reduce oxalate absorption. Dark green leafy vegetables, nuts, seeds, and whole grains are excellent sources of magnesium.
Prescription Medications
In some cases, medications like potassium citrate or thiazide diuretics might be prescribed to help manage oxalate levels, especially if you have a history of kidney stones or other related health issues.
Monitoring Your Progress
Keeping track of how your body responds to dietary and lifestyle changes is essential. Here are some ways to monitor your progress:
Keeping a Food Diary
Maintaining a food diary can help you track your oxalate intake and identify any patterns or triggers that might worsen your symptoms. Note down what you eat, how much you eat, and how you feel afterward.
Regular Check-ups
Routine medical check-ups are crucial for monitoring your ovary and kidney health. Make sure to follow up with your healthcare provider regularly to adjust your care plan as needed.
Staying Informed
Keeping yourself updated with the latest research and information on oxalates and menopause can help you make informed decisions. Trusted sources such as peer-reviewed journals, reputable health websites, and professional guidance are invaluable.

Conclusion
Managing oxalates during menopause can be challenging, but with the right knowledge and strategies, you can navigate this stage of life more comfortably. By moderating your intake of high-oxalate foods, adopting beneficial cooking methods, staying hydrated, incorporating probiotics, and making overall lifestyle changes, you can mitigate the risks associated with oxalates. Regular medical check-ups, personalized nutrition counseling, and a transparent dialogue with your healthcare provider will further assist you in maintaining optimal health. Remember, menopause is a significant transition, and taking proactive steps to manage your health can lead to a more fulfilling and symptom-free experience.